The first hip replacement performed through the anterior approach was by Robert Judet in 1947 at Garches Hospital in Paris. Today Thierry Judet, the son of Robert Judet continues to use this approach for hip replacement. Prof. Thierry Judet, Chief of Orthopedics at Garches, has used this approach for over 20 years and more than 2000 cases. It has been the preferred technique for primary and revision hip replacement at Garches since 1947.
In 1981, Dr. Joel Matta traveled to Paris to study acetabular and pelvic surgery. He learned the procedure at that time, but did not pursue it further because of his interest in pelvic and acetabular fractures. In 1996, while Dr. Matta was practicing in Los Angeles, a patient who had an anterior approach hip replacement in France approached him with severe arthritis of the other hip. He reconsidered the procedure and began performing the operation. At first, he replaced 20 to 30 hips per year, but now performs over 500 cases yearly. Dr. Matta has been a pioneer for advancement of the anterior approach here in the United States. He accepts one orthopaedic surgeon per year to become his fellow. Dr. Yerasimides went to Los Angeles in 2005 for one year, mentoring under Dr. Matta and assisting on all surgeries.
The typical incision is about 4 inches long on the front of the hip varying slightly in length depending on the size of the patient. The smaller incision is more cosmetic, but adequate for implanting the artificial hip parts. The anterior approach works well because the hip joint is closer to the skin in the front and covered by a thinner layer of muscle and fat than from the back (posterior) or side (anterolateral). Almost all patients regardless of size, shape or age are candidates for this procedure.
The posterior approach to the hip is the most common approach for hip replacement, which exposes the hip joint by splitting the gluteal muscles and detaching other important muscles from the femur. The anterolateral approach, which is also commonly used, also requires detachment of important muscle groups from the femur. The anterior approach goes between muscles to expose the hip joint, leaving all muscles attachments to the femur intact.
An artificial hip depends on the muscles around the hip for stability. With the anterior approach, muscles are left intact, giving immediate stability to the hip after surgery. More traditional hip replacement techniques require periods of strict precautions after surgery to assure the artificial hip will not dislocate. These precautions commonly include limits on flexion of the hip requiring elevated toilet seats and chairs. Patients are also instructed to avoid crossing legs or tying shoelaces. Since the anterior approach preserves muscle attachments, dislocation precautions are not needed. Patients are encouraged to use and position the leg in any manner avoiding the cumbersome restrictions. This accelerates rehabilitation and decreases the hospital stay after surgery.
Along with dislocation risks, leg length inequality has long been a problem with hip replacement surgery. With the anterior approach, the patient lies on their back during the surgery. In this position, fluoroscopy is used to determine leg lengths, correct position and proper sizing of the implants. This ensures that every patient leaves the operating room with the artificial hip components most suited for their body.
With all the advantages the anterior approach provides, some patients ask why orthopaedic surgeons do not commonly use it across the country. The main reason is lack of training in this particular approach. Orthopaedic surgeons in the United States are routinely taught the posterior and anterolateral approaches for hip replacement, but very few know the anterior approach. The other two approaches have been used for many years by many surgeons and are felt to be fundamentally sound for total hip replacement. This is true and these approaches are very good, but both require cutting natural muscle attachments that can lead to increased dislocation rates and longer rehabilitation compared to the anterior approach. Another obstacle for many surgeons with the anterior approach is the orthopaedic table. A special table is used to position the femur during surgery. Without the table, the surgery can be extremely difficult to perform. Because the table allows the procedure to be performed with the patient lying supine (on back), both hips can be replaced in the same operative setting for those patients with severe bilateral hip arthritis.
Typically, patients are seen by physical therapists in the hospital for gait training and functional activities. Full weight bearing is allowed and patients can go home after achieving basic therapy goals. In general, additional physical therapy is not required as walking and general activity is adequate. If additional therapy is needed, it can be provided on an outpatient basis. Again, there are no dislocation precautions after surgery. Patients are allowed to bend, twist or cross the legs in any position that is comfortable. Patients are commonly discharged home 1-3 days after surgery.

On x-ray, the hip joint space is completely lost (bone on bone) and bone spurs have formed, demonstrating severe arthritis.

The diseased femoral head is removed and the acetabulum is prepared with a “reamer.” The reamer removes the diseased acetabulum and creates a perfectly hemispherical place to implant the new artificial cup.

The artificial cup is press fit into the reamed acetabulum. X-rays are used to confirm good positioning of the cup.

Trial implants are placed in the femur and x-ray images are taken. To assure the proper positioning of implants and leg length, an image of the normal hip is compared with an image of the trial implants of the operated hip.

The films are overlapped to confirm the trial implants sizes will reproduce the proper leg length and hip position. Adjustments are made if necessary before the final hip replacement components are implanted. This process minimizes possible leg length discrepancy.

An x-ray of the same hip after joint replacement shows the artificial implants in place. The rough, diseased joint has been replacement with a smooth gliding artificial joint, relieving pain and regaining motion.

What does hip arthritis feel like?
- Pain in the groin or front of the hip
- Pain radiating down the front of the thigh and shin
- Difficulty putting on socks and shoes
- Difficulty getting into the car
- Difficulty when standing from a chair
- Pain while lying in bed
- Weakness of the hip muscles and limping
When should you consider hip joint replacement?
There is no textbook answer to this question. The answer lies within each person on an individual basis. The correct time is when the pain is severe and prevents you from enjoying normal life activities. Traditionally, orthopaedic surgeons have encouraged patients to wait as long as possible before having surgery. With new implant designs and improved longevity, patients can have hip replacement earlier, before losing valuable years “waiting” until they were older.
What should you expect from hip replacement?
The vast majority of patients undergoing hip replacement experience good results with elimination of pain, increased flexibility and return to normal activity. With anterior approach hip replacement, you will be able to return to activity without restrictions. Data we currently have from hip replacements performed 15-20 years ago show us that survival rate is approximately 95% at 15 years and 70% at 20 years. Hip replacement is, in fact, one of the most successful surgeries in all fields of medicine. It has proven to have a very high patient satisfaction rate with a very low complication rate.
What should you do to prepare for hip replacement?
Once you have decided to discuss anterior approach hip replacement, call my office for a consultation date. If you have a date already, make arrangements for time off work. The duration of time will vary from person to person and specific occupation. It is also preferable if you have someone with you after surgery. This is only necessary until you are mobile enough to be independent. If you smoke, stop. Smoking significantly increases your surgical risks and complications.
Bactroban Nasal Ointment
We will giving you a prescription for Bactroban (Mupirocin) ointment to apply to your nasal passages to prevent staph infections during surgery.
Directions for use: Apply generously inside each nostril with a separate Q-tip for each nostril and each application. (you should be using 2 Q-tips for each application) This is done twice a day starting 5 days before your surgery, so that you finish the last application the night before surgery.
Hibiclens Body Wash
This is given to also help reduce skin bacteria at the incision site. Wash the affected body part (entire limb) once or twice a day for 5 days prior to surgery. You can also use the morning of your surgery.
Post operatively we recommend that you use dial antibacterial soap to gently clean your incision. You will be allowed to shower 24-48 hours after surgery and begin washing the incision. DO NOT take a tub bath or soak the incision for 2-3 weeks post operatively.
What should you expect on the day of surgery?
Arrive at the hospital when instructed. Make sure you have not had anything to eat or drink since before midnight the night before. After surgery, you will spend 1-2 hours in the recovery room before going to your hospital room. You will have a pain medicine pump to use as needed. You will also have medications available for nausea and sleep as needed.
Day of Surgery
You will go to the recovery room for 1.5-2 hours after surgery. You will be allowed to wake up and have family or friends come in to see you after you are awake. You will have a pain medicine pump started to use as needed. Once you are awake, you will be transported up to your room. All rooms are private and have a couch that pulls out to a bed for any family or friends that want to stay with you.

Hospital Stay
You will spend anywhere between 1-3 days in the hospital. A physical therapist will see you twice daily for simple gait and stair training. You will use a walker or single crutch in the hospital. There will be no dislocation precautions and you will be allowed to put as much weight on the leg as tolerable. You will have pain pills and IV pain medicine if you need them. The catheter and drain will be pulled the day after surgery. You will have an x-ray taken of your pelvis the day after surgery. A blood thinner will be started in the hospital to prevent development of a blood clot.
The Incision
Your incision will be closed with absorbable suture under the skin. The top of the incision is covered with “glue” called Dermabond which provides a watertight seal. After the drain is pulled, there will be a hole in the skin that will drain for up to 3-4 days. You will be allowed to shower immediately after the dressing is removed, allowing water to run over the incision. Please do not sit in a bath, hot tub or pool for 3 weeks after surgery.
Swelling/Bruising
It is normal for the operative leg to swell after surgery. You may even have swelling past the knee into the ankle and foot. It is a good idea to wear compression stockings for the first 2-3 weeks to help control the swelling and improve circulation. If the swelling becomes severe or the calf painful, please call because it could be the sign of a blood clot. It is also common to have bruising along the side or front of your thigh. This may extend to the knee as well but will resolve and is a normal expectation after surgery.

Physical Therapy
You will be seen twice daily by a physical therapist in the hospital. They will start you walking with the aid of a walker and graduate to crutches or cane as your balance and strength improve. Unless told otherwise, you are allowed to put as much weight on the artificial hip as tolerated. There will be no dislocation precautions, so you are allowed to bend, squat and twist as comfort allows. You may sleep on your stomach or side if you prefer. Therapy will be arranged to come to your home after discharge.
**Restrictions**
There are no restrictions unless specifically identified by myself. You are allowed full weightbearing and have no dislocation precautions. Please restrict climbing flights of stairs for 7-10 days after surgery. Limit high impact activities such as running for 3 months to allow the implants to fully heal to bone.

Follow Up
Your first follow up appointment will be 6 weeks after surgery. The hospital staff should make an appointment for you before discharge and provide you with a date and time. If everything is progressing well and the x-ray looks good at 6 weeks, we will start yearly follow up appointments at that time.

Infection
Any time an incision is made and the inside of the body exposed, an infection can occur. You will receive antibiotics before and after surgery to prevent a surgical wound infection from developing. If an infection develops in an artificial hip, the implants may need to be removed for a period of 6-8 weeks while antibiotics are given. Re-implantation occurs after this period, but recovery is delayed significantly.
Bleeding
Most patients undergoing hip replacement will not lose enough blood to require blood transfusion. Those undergoing bilateral hip replacements are at increased risk for requiring blood transfusion. If you develop a large collection of blood under the skin, you may have to return to the operating room to have the wound hematoma evacuated.
Nerve Injury
It is extremely rare to have a major nerve injury during anterior approach hip replacement. The main nerve at risk is the lateral femoral cutaneous nerve, which gives you sensation on top of the thigh. This nerve is very rarely injured. Some patients will have numbness to the side of the incision from small skin nerves being cut in the approach. This area is usually small and will continue to decrease in size over 2-3 months.
Leg Length Inequality
This is one of the most common patient complaints following hip replacement surgery. The anterior approach addresses this issue by using fluoroscopic x-rays in the operating room to ensure equal leg length while adjustments can still be made. Even with x-ray assistance, small leg length differences can occur but are rare.
Dislocation
Dislocation can occur with extremes of movement, especially during the first 2-3 months after surgery. The risk of dislocation is significantly reduced using the anterior approach to the point that no dislocation precautions are used after surgery. If a dislocation occurs, you will have to return to the hospital to have your hip put back in place.

Fracture During Surgery
It is possible to fracture the femur bone while implanting the femoral stem of the artificial hip. The component is wedged tightly into the canal of the femur taking care not to use too much force, but on occasion, a crack in the bone will occur. If this does occur, we can expect the bone to heal without problem. If this happens, restrictions may be placed on weight bearing after surgery.
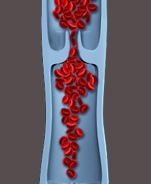
Blood Clots
A blood clot, or deep vein thrombosis (DVT), is a known postoperative complication of joint replacement. If a DVT develops, it can travel to the lungs causing a pulmonary embolus (PE) which is life threatening. All patients after hip replacement are placed on blood thinners for this reason. You will have compression stockings and leg compression boots in the hospital to increase circulation. Symptoms of DVT/PE include new or unusual leg or calf pain, chest pain and shortness of breath. If you experience any of these symptoms at home, please consult with a medical doctor.

Increased Risk for Smokers
Smoking greatly increases your chances of infection, wound complications, and deep vein thrombosis. Smokers also are at increased risk for pulmonary complications in the hospital. If you smoke, it is in your best interest to stop before undergoing hip replacement surgery.